Transient epileptic amnesia (TEA) is a rare form of temporal lobe epilepsy that is characterized by recurrent observable episodes of transient amnesia that spare cognitive functions other than memory and are corroborated by epileptiform abnormalities in electroencephalography (EEG), clinical manifestations of epilepsy, or a good response to antiseizure therapy.1 When clinical features of epileptic events and EEG abnormalities are absent, TEA may be misdiagnosed as transient global amnesia (TGA) due to this condition exhibiting similar clinical features. The diagnosis of TEA is often delayed from several months to more than 10 years after the onset of symptoms.2,3 Here we present the case of a middle-aged female who over 3 years experienced four episodes of amnesia with durations of at least several hours.
CASE
A 54-year-old female visited the hospital with a complaint of experiencing four distinct episodes of amnesia over 3 years. The symptoms had a sudden onset, and the episodes lasted 2-12 hours. During these episodes the patient displayed a characteristic behavior, typically asking repeatedly, ‘what time is it now?’ and ‘what am I doing here?’ Her husband and son reported they did not observe any abnormalities other than repeated questions. Prior to each episode, the patient reported that she experienced significant family-related stress. The patient had previously been diagnosed with TGA and was taking an antiplatelet medication. Brain magnetic resonance imaging (MRI) performed during each episode did not reveal any abnormalities. The patient had no history of hypertension, diabetes, hyperlipidemia, or heart disease. She did not consume alcoholic beverages or smoke cigarettes. No relevant risk factors for epilepsy such as febrile seizure, head injury, intracranial infection, or a family history of epilepsy were reported. On the 10th day after the last event, the patient’s vital signs were stable and the findings of a neurological examination were normal. The patient was right-handed, had graduated from university, and did not complain of any cognitive decline. The patient scored 30 points on the Korean version of the Mini Mental Status Examination. Blood tests, including of thyroid function, produced normal results.
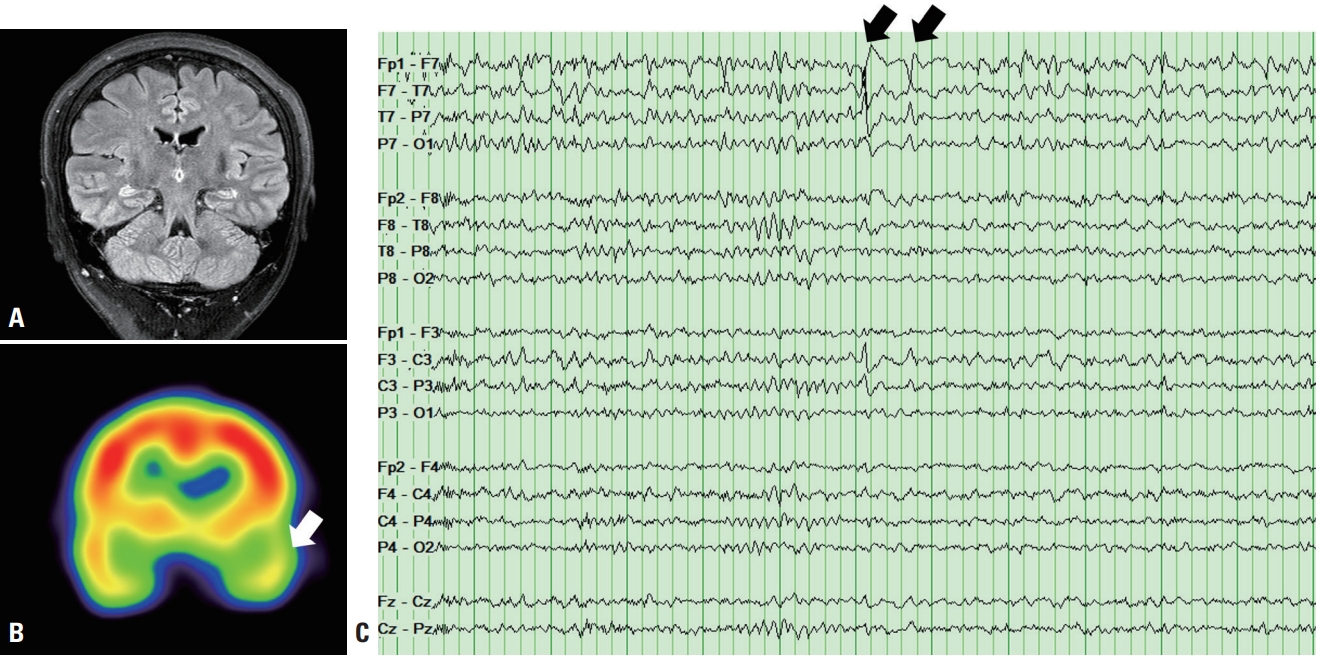
Given the patient’s recurrent memory loss, it was necessary to differentiate epileptic amnesia from other causes. Brain MRI performed to check the temporal lobe, including the limbic system, produced normal results (Fig. 1A). However, technetium-99m-ethyl cysteinate dimer single-photon-emission computed tomography revealed slightly decreased perfusion in the left anterior temporal area (Fig. 1B). EEG revealed sharp waves in the left temporal region (Fig. 1C). We conducted a repeat extensive interview with the patient as well as her husband and son to identify any signs or symptoms suggestive of epilepsy. The patient's son recalled that she once had expressed lightheadedness just before the symptom began. After the symptom began, her speech became slightly slow and her face appeared dazed. The patient was diagnosed with TEA and so she was prescribed lamotrigine at 100 mg twice daily. She has been symptom-free for more than 30 months.
DISCUSSION
TEA is a type of late-onset temporal lobe epilepsy that is characterized by short episodes of memory loss for up to 1 hour, frequent occurrence, and interictal subjective cognitive decline.1-3 Although the pathophysiology of TEA is unclear, acute transient anterograde amnesia is thought to result from a combination of abnormal epileptic discharges in the temporal lobe and dysfunction in the hippocampus and other legions involved in memory formation and storage.4 A study of 50 patients with TEA found that 82% had symptoms lasting less than 1 hour, with the remaining 18% having longer episodes lasting from 2 to 24 hours.1 Additionally, eight of the nine patients with longer episodes had epileptic features such as olfactory aura, generalized tonic seizures, and automatism.1 In Korea, two cases of TEA have been reported with symptom onset within a few minutes, repeated episodes over a short period, and predominantly occurring in the morning shortly after waking up.5 In contrast to the typical TEA symptoms, the present case experienced symptoms lasting at least 2 hours without clear findings suggestive of an epileptic seizure.
While TGA is generally considered a singular occurrence, recurrence is observed in 3-26% of patients and is more frequent in those with a history of depression or head injury or a family history of dementia.6,7 The present case had no history of depression or head injury, or a family history of dementia. TGA is primarily diagnosed based on exclusion of other causes. Notably, like TGA, TEA is often associated with normal or nonspecific findings in brain MRI.2,3,6
The peculiarities of this case can be summarized as follows: 1) despite the relatively long symptom duration, there were no signs suggestive of epilepsy, which usually accompany long-lasting symptoms; 2) there were no symptoms of cognitive decline during the interictal period; and 3) the symptoms appeared relatively infrequently over a long period of time. Although epileptiform discharges are not present in TGA, slow waves can often be observed in the left or both temporal lobes.8
This case indicates that TEA should be included in the differential diagnosis of memory loss in adults. The possibility of TEA should be considered in cases with pure memory loss, and detailed history-taking targeting epileptic origins along with repeated EEG tests should be conducted when symptoms appear repeatedly. The role of EEG as a critical diagnostic tool in TEA and its clear response to antiseizure medications should be emphasized.