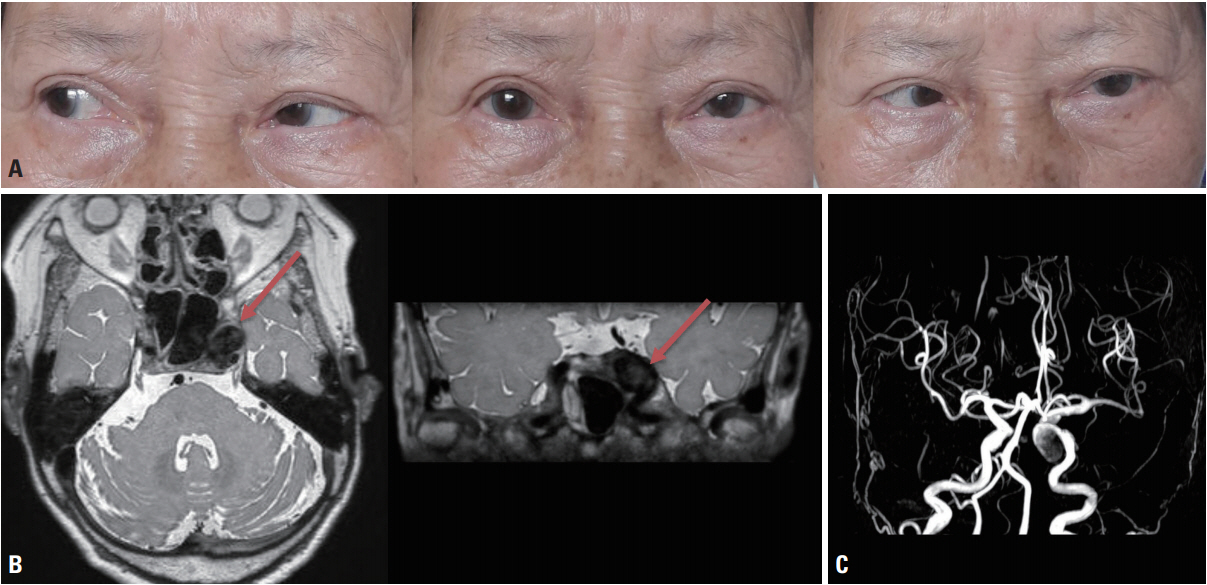
An 80-year-old female was admitted to our hospital with diplopia that had first appeared 3 weeks previously. She did not complain of headache, ocular pain, or tinnitus. A neurologic examination revealed limitations in lateral gaze in the left eye, which suggested left abducens nerve palsy (Fig. 1A). No other abnormalities were found in cranial nerve examinations, such as in pupil size or light reflex. We performed serologic testing, including complete blood count, hemoglobin A1C, and the thyroid function test, and the results were within the normal limits. The patient underwent brain magnetic resonance imaging, which revealed a large cavernous aneurysm in the left internal carotid artery (ICA) originating at the left cavernous sinus (Fig. 1B). This aneurysm compressed the cavernous sinus segment of the left abducens nerve, causing abducens nerve palsy. Digital subtraction angiography confirmed a 2.37 ├Ś 1.71 cm aneurysm in the cavernous portion of the left ICA (Fig. 1C). The patient underwent coil embolization using the stent-assisted technique, and her gaze symptom had improved 4 months later.
There are various causes of isolated abducens nerve palsy, but an aneurysm origin is very rare.1,2 A recent prospective multicenter study investigated the patterns and etiologies of acquired ocular motor nerve palsy (OMNP) in 298 patients. Abducens nerve palsy was the most common type of OMNP in these patients (40%), but none of them had isolated abducens nerve palsy produced by an aneurysm.2
The abducens nerve comes from the junction of the pons and medulla and passes through the subarachnoid space and cavernous sinus before entering via the superior orbital fissure. In a cavernous sinus, the abducens nerve lies beside the sheath of the ICA on the medial side. The dorsal meningeal artery that supplies the abducens nerve comes from the meningohypophyseal trunk.3 As a result, aneurysm or dissection of the cavernous ICA could produce abducens nerve palsy by direct compression or via interruption of the blood supply to the nerve.4 Clinicians must therefore consider ICA aneurysms when patients present with isolated abducens nerve palsy.