Optic nerve sheath meningioma mimicking optic perineuritis
Article information
Abstract
Tram-track and doughnut-shaped enhancements of the optic nerve sheath in axial and coronal magnetic resonance imaging (MRI) views, respectively, play crucial roles in the diagnosis of optic nerve sheath meningioma (ONSM). However, this finding is not specific to ONSM since it can also be observed in optic perineuritis (OPN). Here we report a 42-year-old female with ONSM who presented with clinical and MRI findings similar to those of OPN.
Optic nerve sheath meningioma (ONSM) presents as characteristic tram-track and doughnut-shaped enhancement of the optic nerve sheath on magnetic resonance imaging (MRI). However, this distinct pattern of optic nerve sheath enhancement can also be observed in other conditions, such as optic perineuritis (OPN).1 OPN is optic nerve sheath inflammation that can lead to loss of vision.2 It has recently attracted interest from neurologists who treat central nervous system demyelinating disorders due to its relevance in myelin oligodendrocyte glycoprotein (MOG) antibody-associated disease (MOGAD).3 MRI and clinical findings play very important roles in OPN diagnosis.2 Here we describe a patient with ONSM who presented with clinical and MRI findings similar to those of OPN.
CASE
A 42-year-old female presented with a 2-month history of painless blurred vision in the left eye. Visual acuity was 20/20 in the right eye and 20/40 in the left eye. There was no dyschromatopsia or relative afferent pupillary defect. Ophthalmoplegia, ptosis, and exophthalmos were not observed. The fundus examination and fluorescein angiography of the right eye showed no abnormalities (Fig. 1A), whereas the left eye showed swelling of the optic disc (Fig. 1B). Notably, no optociliary shunt vessels were found in the left eye (Fig. 1B). The Humphrey visual test of perimetry revealed normal results in the right eye (Fig. 1C), but the left eye showed slightly enlarged blind spots (Fig. 1D). The full-field pattern-reversal visual evoked potentials revealed the absolute values of the bilateral P100 latencies to be in the normal range, but there was an interside difference of significant latency prolongation on the left side. MRI revealed diffuse circumferential thickening and enhancement in the left optic nerve sheath, with a tram-track and doughnut-shaped appearance in axial and coronal MRI views, respectively (Fig. 2A, B). Computed tomography (CT) revealed no calcification around the left optic nerve (Fig. 2C). A cerebrospinal fluid examination revealed normal cell counts and protein levels, and did not detect oligoclonal bands. Antibodies against aquaporin-4 and MOG were not detected. Serologic test results were negative for syphilis, human immunodeficiency virus, and toxoplasma, and levels of serum markers for immunity and inflammation were normal, including antineutrophil cytoplasmic antibody, immunoglobulin G (IgG), and erythrocyte sedimentation rate. CT of the neck, chest, abdomen, and pelvis revealed no evidence of sarcoidosis or malignancy. OPN and ONSM were provisionally diagnosed based on characteristic MRI findings. The patient was treated using high-dose intravenous methylprednisolone (1,000 mg/day) for 5 days, which did not achieve any noticeable improvement. Follow-up MRI at 10 months after the initial investigation revealed persistent thickening and enhancement of the left optic nerve sheath (Fig. 2D, E). The patient was finally diagnosed with ONSM based on the painless presentation, lack of response to steroids, and long-standing persistent enhancement of the optic nerve sheath. Fortunately, the patient had experienced no deterioration in vision during the 22-month follow-up period after onset. Radiation therapy will be considered in the future if the symptoms worsen.

Fundus examination revealing normal findings in the right eye (A) and a swollen optic disc in the left eye (B). Optociliary shunt vessels were not detected in the left eye (B). The Humphrey visual test of perimetry produced normal findings in the right eye (C) and slightly enlarged blind spots in the left eye (D).
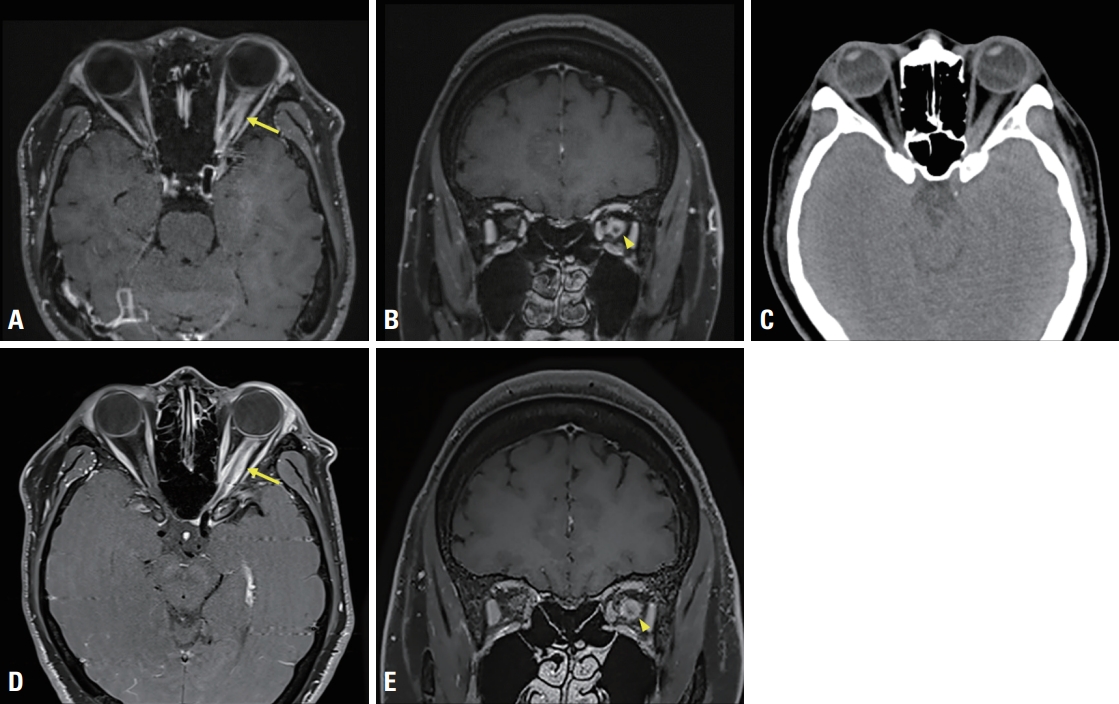
Gadolinium-enhanced T1-weighted MRI images reveal diffuse circumferential thickening and enhancement in the left optic nerve sheath with tram-track (arrow) and doughnut-shaped (arrowhead) appearance in axial (A) and coronal (B) MRI views, respectively. Calcification was not observed around the left optic nerve in noncontrast computed tomography (C). Follow-up MRI images at 10 months after the initial investigation reveal persistent thickening and enhancement of the left optic nerve sheath (arrow, D; arrowhead, E). MRI, magnetic resonance imaging.
DISCUSSION
OPN is an important clinical presentation for distinguishing MOGAD from multiple sclerosis or neuromyelitis optica spectrum disorder.2 Tram-track and doughnut-shaped enhancements of the optic nerve sheath in axial and coronal MRI views, respectively, play crucial roles in OPN diagnosis.3 However, this finding is not specific to OPN since it can also be observed in ONSM.3,4
ONSM is sometimes accompanied by nerve sheath calcification and optociliary shunt vessels on CT and fundus examination images, respectively, which can help in differentiating it from OPN.3,4 However, in the absence of these findings, as in our patient, it is difficult to differentiate ONSM and OPN using MRI findings alone. Unlike OPN, ONSM manifests as painless visual loss, does not respond to steroids, and exhibits persistent optic nerve sheath enhancement.4 Moreover, the inflammation of MOG-IgG-associated OPN in patients often extends into the surrounding orbital fat tissue outside the optic nerve sheath,5 which contrasted with the MRI finding of the present case. These characteristics can provide important clues for differentiating ONSM from OPN.
Other possible conditions that present with optic nerve sheath enhancement on MRI were also considered since the lesion was not biopsied in our case. The specific MRI signs undoubtedly played the most important role in the differential diagnosis; the possibility of other tumorous and tumor-like conditions1 such as glioma, lymphoma, sarcoidosis, inflammatory orbital pseudotumor, and IgG G4-related disease were also excluded based on the clinical presentations, lack of response to steroids, and blood test results.
The clinical and radiologic features of ONSM and OPN may overlap, resulting in late diagnosis and treatment. Clinicians should consider this in the differential diagnosis of patients with optic nerve sheath enhancement.
Notes
Conflicts of Interest
The authors have no conflicts of interest to declare.
Acknowledgements
This research was supported by KBRI basic research program through Korea Brain Research Institute funded by Ministry of Science and ICT (23-BR-03-02).
