Quantitative sudomotor axon reflex test (QSART) as a diagnostic tool of small fiber neuropathy
Article information
Abstract
Small fiber neuropathy is a painful neuropathy that cannot be assessed using nerve conduction studies. A skin biopsy and quantitative sensory testing (QST) are the gold standards for small fiber neuropathy diagnosis. However, a skin biopsy is invasive and commercially unavailable in Korea. QST is a method involving a thermal threshold, but its results can be affected by cognition as well as lesions of the central nervous system. Quantitative sudomotor axon reflex test (QSART) is a quantitative method of assessing sweat glands innervated by small fibers. In this review, we assessed the utility of QSART in evaluating small fiber neuropathy.
INTRODUCTION
Small fiber neuropathy is a type of painful sensory neuropathy.1 Although its exact prevalence is not known, it is considered to have relatively high morbidity among neuropathies.2,3 A survey in the Netherlands estimated the small fiber neuropathy prevalence at only 53 per 100,000 persons, which seems to be a considerable underestimation.4,5 Fibromyalgia is a well-recognized chronic pain disorder with a widespread burden whose prevalence in the general population is about 2%. Recent skin biopsy studies found that 40–60% of patients with fibromyalgia had a reduced intraepidermal nerve fiber density (IENFD).5,6 In other words, at least regarding the cutaneous pathology, about half of patients with fibromyalgia also present with small fiber neuropathy. Since small fiber neuropathy can be caused by various common systemic disease such as diabetes mellitus, impaired glucose tolerance, chronic kidney disease, hypothyroidism, Sjogren syndrome, hepatitis C, paraproteinemia, vitamin B12 deficiency, alcoholism, etc. the prevalence is estimated to be high affecting millions of people worldwide.7-9
Small fiber neuropathy is a disease of the small-diameter nerve fibers that consist of thinly myelinated Aδ or unmyelinated C nerve fibers. Small nerve fibers do not convey motor functions nor proprioception, but instead are responsible for somatic pain and temperature sensations, and autonomic function.3 The small-diameter dermal autonomic nerve fibers consist of pilomotor, vasomotor, and sudomotor fibers.10 Sensory symptoms of small fiber neuropathy include burning and stinging pains, and abnormal sensation. It can also cause autonomic dysfunction especially in cutaneous autonomic function such as sweating, because sudomotor fibers consist of small-diameter sympathetic nerve fibers.11 If a lesion is confined to only the small nerve fibers, the patient still exhibit normal muscle strength and deep tendon reflexes during neurological examinations. A nerve conduction study (NCS) is the most important tool for evaluating peripheral nerves, but it can also only assess large-diameter nerve fibers and thus cannot be used for confirmative small fiber neuropathy diagnoses.7,12
DIAGNOSING SMALL FIBER NEUROPATHY
Diagnostic criteria for small fiber neuropathy have been reported, and a skin biopsy is often regarded as the gold-standard tool for small fiber neuropathy diagnosis.5,13 In several studies, skin biopsy presented high sensitivity (74–90%) and specificity (64–90%) for small fiber neuropathy diagnosis. In cases of suspected small fiber neuropathy based on symptoms and signs, the first diagnostic step is an NCS to confirm that the symptoms of the patients were not caused by large fiber neuropathy, and small fiber neuropathy can be diagnosed through either quantitative sensory testing (QST) or IENFD with a skin biopsy.12 QST is a test that relies on the judgment of its subject, and it therefore has the inherent limitations that it cannot be applied to patients with dysfunctional cognition or attention deficits, and that intentional errors can also occur. Furthermore, abnormal findings in QST do not always indicate the presence of lesions in small nerve fibers, and lesions of other somatosensory nervous area such as the central nervous system cannot be ruled out.3
Small fiber neuropathy diagnosis using IENFD verification is an objective method and a very useful tool. A skin biopsy can be used to investigate dermal tissue that contains a cutaneous autonomic structure and adnexa, and also the dermo-epidermal junction using IENFD.14 However, this method also has some limitations. A skin biopsy is a minimally invasive, safe specimen-obtaining procedure that often does not need sutures.15 Although minimally invasive, minor bleeding is inevitable during biopsy and the healing time is about 1 week. Handling and staining of the cutaneous specimen are also labor-intensive, time-consuming, and can be expensive. Furthermore, this method cannot be used in clinical settings because it is not commercially available in Korea. Other tools are therefore needed for small fiber neuropathy diagnosis.
SMALL FIBER NEUROPATHY AND SUDOMOTOR FUNCTION EVALUATION
Autonomic involvement occurs in many peripheral neuropathies including small fiber neuropathy. Pain and autonomic dysfunction are the most representative symptoms of small fiber neuropathy. The targets of common skin biopsy and QST are anatomical or functional assessments of pain and temperature; these methods therefore lack methods for cutaneous autonomic function evaluation, which is another important problem in small fiber neuropathy.
Sweat glands are exocrine glands, and most sweat glands in humans are classified as apocrine or eccrine glands.16 Apocrine sweat glands are densely distributed on hairy skin in close proximity to sebaceous glands in most mammals. Humans have less densely distributed apocrine glands than other mammals, and are often restricted in the axillary fossa, eyelids, areola, and the pubic and perineal regions. Unlike in other mammals, human eccrine glands are widely distributed in both the hairy and glabrous skin, except for the regions with apocrine glands.16 Sweating at the palm or sole is associated with emotional conditions such as fear or anxiety. In contrast to glabrous skin, the main role of eccrine glands in hairy skin is body temperature regulation.16 Eccrine glands are innervated with sympathetic nerves. However, in contrast to most postganglionic sympathetic nerves, acetylcholine is the neurotransmitter of sudomotor sympathetic nerves to eccrine glands, possibly because cholinergic vasodilatation would be helpful in inducing sweating.17
Sudomotor function is one of the most important functions of the cutaneous autonomic system, and several tools have been used to assess it. Methods for testing sudomotor function include sympathetic skin response, electrochemical skin conductance (ESC), the thermoregulatory sweat test (TST), and the quantitative sudomotor axon reflex test (QSART).18-20 Each tool has its own advantages and disadvantages, but only QSART can evaluate postganglionic sympathetic functions of the pure small nerve fibers of the dermal tissue.21
QSART
Low first introduced QSART in the Mayo Clinic in 1983, which has achieved widespread clinical use. QSART is a method for evaluating postganglionic sympathetic cholinergic sudomotor function.22,23 The eccrine glands of hairy skin are the sources of QSART responses, and that test measures the axon-reflex-mediated evaporated sweat response. The Q-Sweat device (WR Medical Electronics, Maplewood, MN, USA) is a commercially available version of the QSART, which is used at several autonomic laboratories as the battery of autonomic function tests. Compared with the QSART from the Mayo Clinic, Q-Sweat results had longer latencies and smaller sweat volumes, which might be associated with ion delivery efficiency, so the physician should interpret the results while referring to the reference material for each method.24
To elicit a sweat response, the axon reflex uses a multicompartment cell and iontophoresis techniques with stimulation using a 10% acetylcholine solution.20 Common test sites are the medial forearm, proximal leg, distal leg, and extensor digitorum brevis muscle at the dorsum of the foot. After stable baseline levels have been reached, a 5-mA current applied for 5 minutes induces iontophoresis with a 10% acetylcholine solution penetrating the skin.25 Acetylcholine penetration stimulates sudomotor fiber endings and elicits retrograde action potentials, and after it reaches nerve branching sites, anterograde propagation occurs in the sweat glands and induces a sweat response (Fig. 1).20 After a latency of 1–2 minutes, the humidity of each multicompartment cell is recorded for 10–15 minutes from baseline and sweat levels can be quantified and displayed. The latency and area under the curve can be measured, but only the area has clinical significance.22,25,26
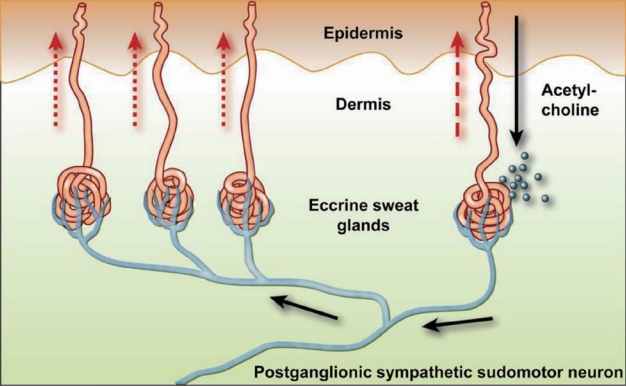
The sudomotor axon reflex. Ten% acetylcholine applied through iontophoresis (shown with the black arrows) bind to muscarinic receptors causing local sweat production (dashed arrows). The action potential travels antidromically and then it reaches nerve branching sites, anterograde propagation reaches to neighboring eccrine sweat gland and induce indirect sweat response (dotted arrows). Reprinted from Illigens and Gibbons20 with permission.
Sweat level is higher in males than in females, and older age is related to reduced sweating, although this age-related reduction was not demonstrated in a Korean study.26 In diseases with sudomotor dysfunction such as polyneuropathy, ganglionopathy, or small fiber neuropathy, the sweat amount decreases according to the QSART. Furthermore, in cases of length-dependent pattern polyneuropathy or small fiber neuropathy, there can be a length-dependent reduction in sweat production, and the distal-proximal sweat-amount ratio is below 1/3.18,27 The autonomic testing battery considers cardiovagal, sudomotor, and adrenergic functions, and it can be scored using the 10-point composite autonomic severity score (CASS).25 In CASS, sudomotor function is tested using either QSART or TST. The sudomotor index in CASS is a score ranging from 0 to 3, and it is calculated using the number of abnormal sites, degree of abnormality (sweat volume <50% of the 5th percentile), and whether a length-dependent pattern presents that is less than 1/3 of the distal-proximal gradient.25
QSART IN SMALL FIBER NEUROPATHY
Skin biopsy of dermal tissue can quantify the sweat gland nerve fiber density (SGNFD). Although the correlation between IENFD and SGNFD is not particularly strong, SGNFD is correlated with the severities of diabetic neuropathy and sudomotor symptoms. An ESC study is another method for evaluating sudomotor function, where an ESC reduction is proportional to IENFD and SGNFD.28,29
Abnormal QSART scores would result from disease or dysfunction from the indirect sudomotor axon reflex arc that consists of the sympathetic C fiber, or the sweat gland itself. QSART may therefore represent the status of small fiber neuropathy. Up to 11% of published diagnostic criteria for small fiber neuropathy, autonomic function tests including QSART are either mandatory or optional components of the criteria.30 Several studies have used the sudomotor function tests of TST or QSART, and found diagnostic sensitivities for small fiber neuropathy of 52–80%.25 In these studies, sudomotor dysfunction included either distal anhidrosis or any other abnormality. Thaisetthawatkul et al.17 suggested diagnostic criteria for the QSART: (1) compatible sensory symptoms without motor weakness or upper motor neuron signs, (2) normal electromyography (EMG)/NCS findings, and (3) at least two abnormalities on the QST, QSART, or skin biopsy. They also proposed a relaxed set of modified criteria for those who cannot obtain QST or can only access the QSART or skin biopsy: (1) sensory symptoms without motor weakness, (2) normal EMG/NCS findings, and (3) abnormal “small fiber” sensory examination results (pin sense) in combination with abnormality in either the QSART or IENFD.17 Cheshire et al.25 reported that the QSART could diagnose small fiber neuropathy with a high accuracy: (1) sudomotor volume <5th percentile at the foot and a length-dependent decrease (sudomotor volume at the foot <1/3 that of the proximal site), or (2) sudomotor volume <5th percentile at the foot and either a history of distal dysesthesia or distal deficit to small fiber sensory modalities observed in a physical examination. While skin biopsies are difficult to use in Korea, autonomic function tests and QST have been relatively popular and can be used; QSART or QST may therefore be of practical help (Table 1).
Other major parts of autonomic function tests can also include diagnosing small fiber neuropathy, but their sensitivities are lower than those of sudomotor tests. The sensitivities of cardiovagal function and sympathetic adrenergic abnormality tests were 28–75% and 0–43%, respectively.21 Although sudomotor evaluation is a useful tool for small fiber neuropathy diagnosis, sudomotor abnormality is independent of a somatic evaluation.27 When applying QSART, QST, and IENFD for small fiber neuropathy, reduced IENFD had a statistically significant relationship with abnormal QSART.27,31 However, linear regression was not applied to the relationship between QSART volume and IENFD, and an abnormal QSART was not related to abnormal pin-prick examination results.27
CONCLUSIONS
Small fiber neuropathy is a relatively common peripheral neuropathy. However, making reliable diagnoses is still challenging, partly because physicians often cannot use all of the diagnostic tools in individual neurological clinic settings. The parameters for small fiber neuropathy diagnosis should include (1) sensory symptoms of small nerve fiber injury, (2) sensory signs of small nerve fiber injury in a neurological examination, (3) absence of abnormal NCS findings suggesting large-fiber involvement, and (4) structural or functional identification of small nerve fiber involvement that may explain the symptoms and signs experienced by the patient.30 This review about 4th component of diagnostic modality and in cases of skin biopsy being unavailable, sudomotor tests such as the QSART could be recommended as diagnostic tools with acceptable reliability and sensitivity if other parameters and length-dependent patterns are supported.
Notes
Conflicts of Interest
The author declares no conflicts of interest relevant to this article.

