
|
| About the Journal |
| Aims and Scope |
| Journal Information |
| Editorial Board |
| Best Practice |
| Subscriptions |
| Contact Us |


|
| About the Journal |
| Aims and Scope |
| Journal Information |
| Editorial Board |
| Best Practice |
| Subscriptions |
| Contact Us |

AbstractUltrasonography is currently being developed as a tool for evaluating peripheral neuropathy. It is one of the painless and least-invasive methods of medical diagnostic testing that yields anatomic views of the nerves and their surrounding structures. Here I first describe the equipment settings and technique for nerve ultrasound along with typical sonographic findings for normal nerves. I then address frequently used parameters for nerve measurements that facilitate diagnoses of focal and generalized neuropathies.
INTRODUCTIONMaking a diagnosis of peripheral neuropathy is supported by electrodiagnosis (EDX). Although EDX is a standard diagnostic test, it has two major disadvantages: (1) the inability to provide anatomic information and (2) discomfort experienced by patients. In contrast, neuromuscular ultrasonography is completely safe and complements EDX well by visualizing both the peripheral nerves and surrounding structures, thereby providing useful information that cannot be obtained using EDX alone. Although this visualization is also possible using magnetic resonance imaging, that technique is expensive and often not readily available. Clinicians can use ultrasound to rapidly scan several nerves of interest and evaluate them in real time. This article introduces peripheral nerve ultrasound and gives an overview of the examination technique, normal sonographic findings for nerves, and key measurements.
EQUIPMENT SETTINGSThe imaging resolution of ultrasonography is directly proportional to the frequency of the transducer, while the depth of penetration is inversely proportional to the frequency.1 A high-frequency transducer is utilized in evaluations of neuromuscular disorders. Frequencies of around 10 MHz are usually sufficient for muscles, while nerve ultrasound requires higher frequencies (usually 12-18 MHz) to achieve optimal imaging. Linear-array transducers are normally used in neuromuscular ultrasound and provide good resolution at the image edges (Fig. 1A). In addition, footprint (hockey stick) transducers are useful for accessing confined areas that are restricted by anatomic structures, such as adjacent bone (Fig. 1B). Moreover, such transducers are small enough to fit within a restricted contact area, such as the hands and feet.
Nerve size measurements and evaluations of the intraneural blood flow are necessary to confirm nerve pathology. The application of power Doppler imaging and software for the measurement of the cross-sectional areas (CSAs) of nerves facilitates these assessments. Current ultrasound systems have multiple preset parameter values that optimize the device settings for different body parts. For example, the musculoskeletal preset is designed to give good contrast resolution and sharp detail in areas with muscles and nerves, and clinicians can access this preset (if available) by simply pressing a button on the ultrasound equipment. Below we consider an ultrasound system that has the basic requirements of a high-frequency linear-array transducer, the ability to measure diameters and CSAs, and the power Doppler imaging mode.
ULTRASOUND SCANNING TECHNIQUESPositionDuring examinations of median and ulnar nerves, the elbow is flexed to 80-90° with the forearm supinated in a seated position (Fig. 2A). In the case of the ulnar nerve, some clinicians prefer a supine position with the elbow flexed at 90° and the hand over the head (Fig. 3A). The median and ulnar nerves are usually first scanned from the wrist. The radial nerve is traced in a seated position with the forearm pronated and the elbow moderately flexed (Fig. 4A). The radial nerve is also evaluated in a supine position with the elbow slightly flexed and the shoulder adducted and internally rotated, so that the examiner can reach the posterior arm. The tracing usually starts from the spinal groove. The fibular nerve is first scanned from the fibular head, and so access is facilitated in the lateral decubitus position. The tibial nerve, which passes down the midline of the popliteal fossa, is imaged best when the patient is lying in a prone position on a bed.
LandmarksThe following anatomic landmarks are useful when performing neuromuscular ultrasound: the median nerve at the wrist is found in the carpal tunnel (Fig. 2B), the median nerve is found between the superficial and deep flexor muscles in the forearm (Fig. 2C), the median nerve is located close to the brachial artery in the upper arm (Fig. 2D), the ulnar nerve at the wrist is located medial to the ulnar artery (Fig. 3B), the ulnar nerve at the elbow is located close to the medial epicondyle (Fig. 3C), the radial nerve courses through the radial groove (Fig. 4B), the brachial plexus is located between the anterior and middle scalene muscles, the fibular nerve goes around the fibular head, and the tibial nerve at the ankle is located close to the posterior tibial artery.2 It is advisable to start scanning from one of these anatomic landmarks. Once the nerve has been identified, it can be traced in the proximal and distal directions to find the region of interest. Although all major nerves can be easily found and visualized using these landmarks, having knowledge of the regional anatomy and topography is crucial in the assessments.
Transducer handlingThe transducer is held perpendicular to the nerve to ensure accurate measurements and the correct resolution. If the transducer is not perpendicular to the nerve, the CSA can be overestimated. It is also important to not apply the transducer using too much pressure when scanning, since compression by the transducer can cause changes in shape, size, and echogenicity. This can be avoided by using generous amounts of ultrasound gel.
SONOGRAPHIC FINDINGS FOR NORMAL NERVESNerves have a distinct architecture consisting of fascicles that are surrounded by the epineurium (Fig. 5A). In a transverse view, the normal echo pattern has a honeycomb appearance because the dark punctuate areas are distributed throughout a hyperechoic background resembling the shape of honeycomb.3 The dark punctuate areas correspond to the nerve fascicles and the hyperechoic background corresponds to the epineurium. However, a normal nerve often appears hypoechoic depending on its type and location. For example, the roots, trunks, and cords normally appear as hypoechoic and the normal ulnar nerve appears hypoechoic at the elbow. Normal nerves are oval to round in shape in the transverse plane, and appear as long tubular structures with a mixture of parallel hypoechoic and hyperechoic lines in the longitudinal plane.
DIAGNOSTIC MEASUREMENTSNerve sizeAccurate measurements of nerve sizes are essential because nerve swelling is the most helpful diagnostic marker for peripheral neuropathy.4 The diameter can be measured on longitudinal images, whereas the CSA, swelling ratio, and flattening ratio can be measured on transverse images. Moreover, averaging multiple measurements made of the same dimension can reduce variability.
The absolute value of the CSA is one of the most reliable parameters for diagnosing focal and generalized neuropathies.5 The CSA is measured by tracing just inside the echogenic rim of the nerve (Fig. 5B).5,6 For the ulnar nerve, positioning the elbow with flexion of more than 90° can decrease the CSA at the elbow, and so using a moderate flexion has been recommended.6 Knowledge of the normal nerve size at a given anatomic site is paramount for nerve ultrasound assessments, and so Table 1 lists the normal reference values of the CSA in the Korean population that have been measured at the sites where compression commonly occurs.7 The reported CSA cutoff value of the median nerve in the carpal tunnel is 9-15 mm2.8 The upper limit of the normal value for the CSA of the ulnar nerve at the level of the medial epicondyle is within the range of 8-10 mm2, which is less variable than that of the median nerve.9
The swelling ratio is defined as the difference between the CSAs at the affected site and an unaffected proximal site of the same nerve. In evaluations of carpal tunnel syndrome (CTS), the swelling ratio is obtained by dividing the CSA of the median nerve at the pisiform level by that at the forearm level. This measurement may be useful for identifying entrapment neuropathy associated with polyneuropathy.10 Because polyneuropathy itself can cause diffuse nerve enlargement, the diagnostic accuracy is higher for the swelling ratio than for the CSA. The swelling ratio may also be less affected by the normal variations of the nerve CSA between individuals. The swelling ratio has differed between studies, with the mean value ranging from 1.34 to 1.53.11-13
Another parameter for evaluating focal compressive neuropathy is the flattening ratio, which is calculated by dividing the largest diameter of a nerve by its smallest diameter. This can be useful for detecting entrapment neuropathy because an affected nerve may show changes from a round or slightly oval shape to a remarkably flattened oval shape at the site of compression. A previous study proposed that a flattening ratio exceeding 3 can be used to diagnose CTS.14
Nerve echogenicityNormal nerve echogenicity appears as a honeycomb pattern induced by a mixture of nerve fascicules and connective tissue. In pathological conditions the nerve becomes hypoechoic, and the fascicular pattern is lost due to increased intraneural edema. However, the normal ulnar nerve also appears hypoechoic at the medial epicondyle due to the arcing course.15 This observation may be helpful when evaluating ulnar nerve pathology in the cubital tunnel. Echogenicity is usually assessed subjectively by visually inspecting images. However, such visual assessments are operator-dependent, which makes objective grading of echogenicity impossible. Recent quantitative assessments of nerve echogenicity performed using different automatic methods have demonstrated the superiority of these methods over subjective evaluations.16-18
Intraneural vascularityThere is no internal blood flow within normal nerves observable in color Doppler imaging, and so any detectable internal vascularity is considered abnormal. Compressive or inflammatory neuropathy can cause vascular congestion that increases the intraneural blood flow. Vascularity is assessed by placing the power Doppler box over the nerve. Nonspecific color signal (noise) may flash unpredictably in the tissue when the imaging gain is increased, but only focal color flow signals synchronized with the arterial pulsation should be interpreted as evidence of blood flow. Similar to echogenicity, vascularity is also assessed subjectively. Quantitative analysis of intraneural blood flow using scientific image processing software has been attempted for diagnosing CTS and stratifying its severity.19
MobilityThe median and ulnar nerves are known to be mobile when the corresponding joint moves in flexion or extension. The median nerve moves within the carpal tunnel when the wrist and fingers perform active flexion. This movement can be observed in real time using a transducer placed at the level of the carpal tunnel, with the mobility rated as full, partial, or absent. Full mobility is defined as the median nerve diving deep into the flexor tendons (Fig. 6), partial mobility is defined when the nerve makes a partial turn but does not dive below the tendons, and absent mobility is defined when no significant movement is detected. Several studies have found that compared with healthy individuals, patients with CTS show only partial or absent motion of the median nerve during joint flexion or extension.20-22 One study assessed the mobility of the median nerve in 160 wrists of healthy participants and observed full median nerve mobility in 78 wrists, partial mobility in 82 wrists, and no mobility in 0 wrists. This suggests that while partial mobility of the median nerve is not uncommon in healthy individuals, the absence of median nerve mobility may be indicative of an abnormality.23
During elbow flexion, the ulnar nerve can move from behind the medial epicondyle. Subluxation involves the partial dislocation of the ulnar nerve from the retrocondylar groove to the tip of the medial aspect of the epicondyle. Dislocation is defined as the movement of the ulnar nerve anteriorly beyond the tip of the medial epicondyle. Such hypermobility of ulnar nerve at the elbow has reportedly been observed in 24.3-47.0% of healthy individuals.6,24 Although repetitive dislocation of the ulnar nerve may contribute to ulnar neuropathy, the causal relationship between hypermobility and ulnar neuropathy is not unclear, and so further investigations are warranted.
CONCLUSIONUltrasonography is often used in combination with EDX to not only facilitate the diagnosis of neuromuscular disease but also to assess its etiology. Although it has been used mostly in the diagnosis of focal neuropathies, the field of ultrasound has expanded to other neuromuscular diseases such as polyneuropathy and motor neuron disease. This article has described the basic elements of neuromuscular ultrasound in order to provide a practical beginner’s guide to neuromuscular ultrasound.
Fig. 1.The two types of ultrasound transducers specialized for musculoskeletal applications: linear array (A) and hockey stick (B). 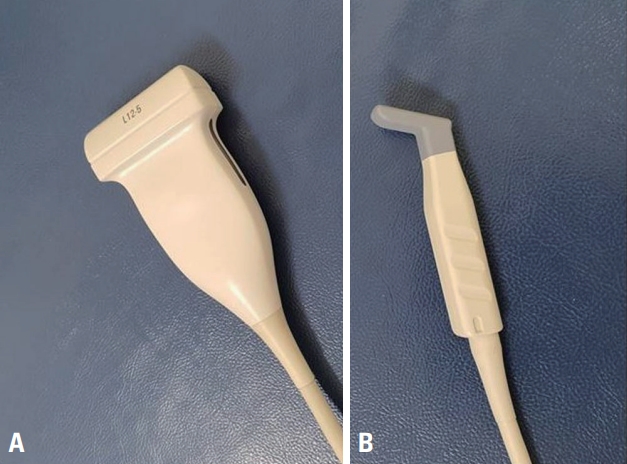
Fig. 2.Normal sonographic anatomy of the median nerve at different levels. (A) The elbow was flexed to 80-90° with the forearm in full supination in a seated position. (B) Transverse image shows the median nerve (arrow) at the proximal tunnel (at the scaphoid-pisiform level). (C) The median nerve (arrow) lies between the flexor digitorum profundus and the flexor digitorum superficialis at the forearm. (D) The median nerve (arrow) lies close to the brachial artery (open arrowhead) at the distal third of the upper arm. BB, biceps brachii; Br, brachialis; H, humerus; fdp, flexor digitorum profundus; fds, flexor digitorum superficialis; fcr, flexor carpi radialis; S, scaphoid; P, pisiform; u, ulnar nerve; a, ulnar artery 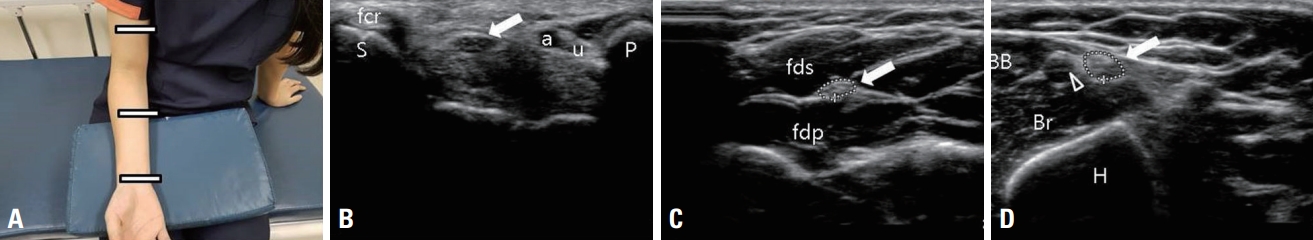
Fig. 3.Normal sonographic anatomy of the ulnar nerve at different levels. (A) The elbow was flexed at 90° in a supine position. (B) Transverse image shows the ulnar nerve (arrow) at the proximal tunnel (at the scaphoid-pisiform level). The ulnar artery and nerve run lateral to the pisiform. (C) Transverse image shows the ulnar nerve (arrow) at the medial epicondyle-olecranon level. m, median nerve; a, ulnar artery; S, scaphoid; P, pisiform; O, olecranon; ME, medial epicondyle. 
Fig. 4.Normal sonographic anatomy of the radial nerve at the spiral groove. (A) The elbow was flexed moderately with the forearm pronated in a seated position. (B) The radial nerve (arrow) lies in close contact with the humerus. t, triceps; br, brachialis; H, humerus. 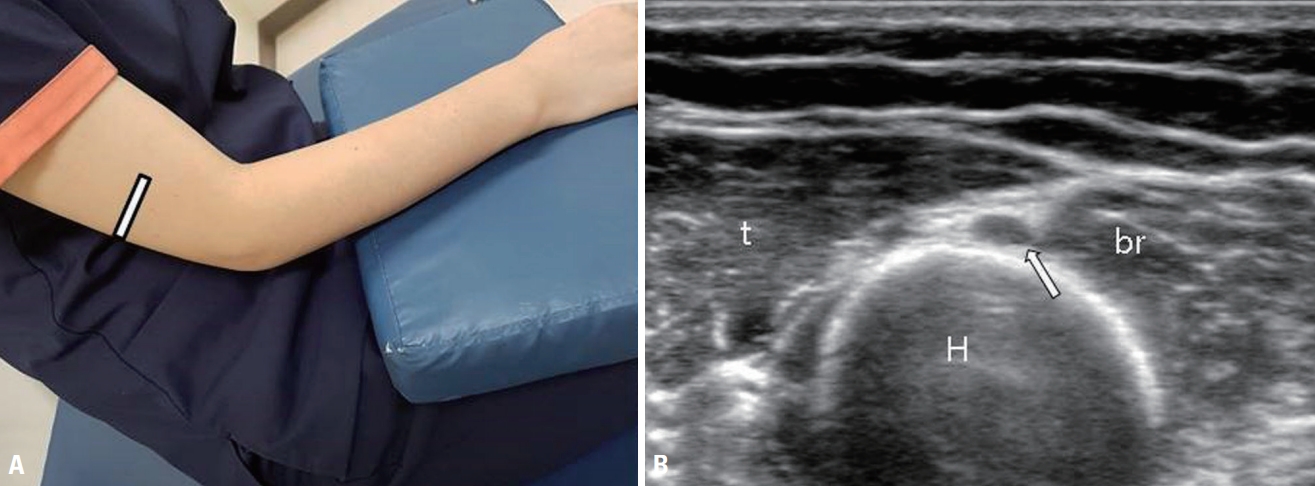
Fig. 5.Normal median nerve. (A) Transverse cross-sectional view of the median nerve (arrow) at the distal wrist crease in a healthy participant. (B) The tracing method performed just inside the hyperechoic rim for measuring the cross-sectional area of the median nerve. fcr, flexor carpi radialis tendon; S, scaphoid; P, pisiform. 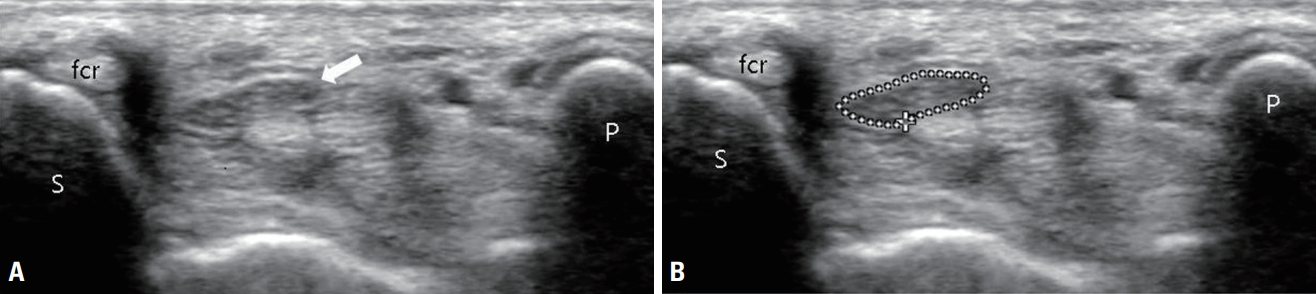
Fig. 6.Ultrasonographic images of the median nerve with full mobility. (A) At rest, the median nerve (arrow) is the most-superficial structure. (B) The median nerve (arrow) dives deep into the flexor tendon when the fingers and wrist are flexed. T, tendon; fpl, flexor pollicis longus; fcr, flexor carpi radialis. 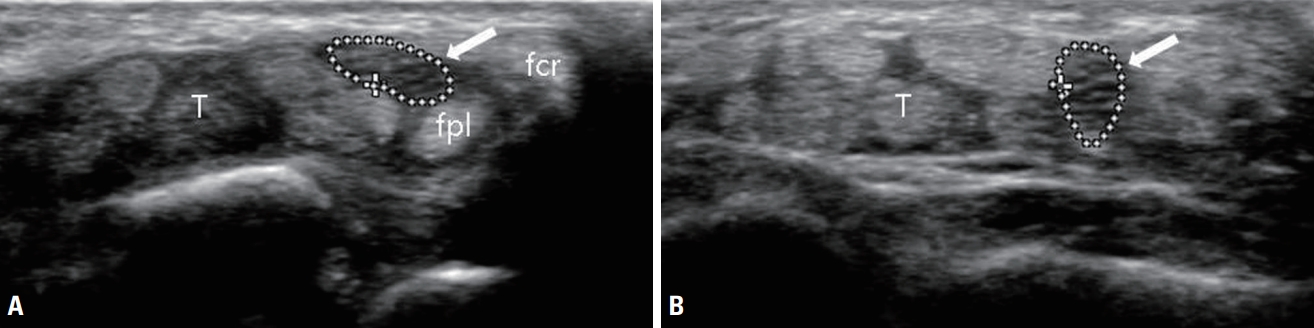
Table 1.Normal reference values of the cross-sectional area The reference range was determined as the mean ± 2 × SD for normally distributed data and between the 2.5th and 97.5th percentiles for nonnormally distributed data. All values are in mm2. Modified from Seok et al.7 with permission of the Korean Neurological Association. SD, standard deviation. REFERENCES1. Walker FO, Cartwright MS, Wiesler ER, Caress J. Ultrasound of nerve and muscle. Clin Neurophysiol 2004;115:495-507.
2. Suk JI, Walker FO, Cartwright MS. Ultrasonography of peripheral nerves. Curr Neurol Neurosci Rep 2013;13:328.
3. Silvestri E, Martinoli C, Derchi LE, Bertolotto M, Chiaramondia M, Rosenberg I. Echotexture of peripheral nerves: correlation between US and histologic findings and criteria to differentiate tendons. Radiology 1995;197:291-296.
4. Duncan I, Sullivan P, Lomas F. Sonography in the diagnosis of carpal tunnel syndrome. AJR Am J Roentgenol 1999;173:681-684.
5. Roll SC, Case-Smith J, Evans KD. Diagnostic accuracy of ultrasonography vs. electromyography in carpal tunnel syndrome: a systematic review of literature. Ultrasound Med Biol 2011;37:1539-1553.
6. Beekman R, Visser LH, Verhagen WI. Ultrasonography in ulnar neuropathy at the elbow: a critical review. Muscle Nerve 2011;43:627-635.
7. Seok JI, Lee SB, Bae CB. Ultrasonographic findings of the normal nerves in common entrapment site; cross-sectional area reference value and normal variant. J Korean Neurol Assoc 2015;33:8-12.
8. Beekman R, Visser LH. Sonography in the diagnosis of carpal tunnel syndrome: a critical review of the literature. Muscle Nerve 2003;27:26-33.
9. Beekman R, Van Der Plas JP, Uitdehaag BM, Schellens RL, Visser LH. Clinical, electrodiagnostic, and sonographic studies in ulnar neuropathy at the elbow. Muscle Nerve 2004;30:202-208.
10. Yoon JS, Walker FO, Cartwright MS. Ultrasonographic swelling ratio in the diagnosis of ulnar neuropathy at the elbow. Muscle Nerve 2008;38:1231-1235.
11. Hobson-Webb LD, Massey JM, Juel VC, Sanders DB. The ultrasonographic wrist-to-forearm median nerve area ratio in carpal tunnel syndrome. Clin Neurophysiol 2008;119:1353-1357.
12. Cho JM, Yoon JS, Kim SJ, Park BK, Lee GH, Jeong JS. Feasibility of ultrasonographic area ratio of median nerve in the diagnosis of carpal tunnel syndrome in Korea. J Korean Acad Rehabil Med 2009;33:627-631.
13. Bathala L, Kumar P, Kumar K, Shaik A, Visser LH. Normal values of median nerve cross-sectional area obtained by ultrasound along its course in the arm with electrophysiological correlations, in 100 Asian subjects. Muscle Nerve 2014;49:284-286.
14. Mallouhi A, Pülzl P, Trieb T, Piza H, Bodner G. Predictors of carpal tunnel syndrome: accuracy of gray-scale and color Doppler sonography. AJR Am J Roentgenol 2006;186:1240-1245.
15. Martinoli C, Bianchi S, Zamorani MP, Zunzunegui JL, Derchi LE. Ultrasound of the elbow. Eur J Ultrasound 2001;14:21-27.
16. Boom J, Visser LH. Quantitative assessment of nerve echogenicity: comparison of methods for evaluating nerve echogenicity in ulnar neuropathy at the elbow. Clin Neurophysiol 2012;123:1446-1453.
17. Watanabe T, Ito H, Sekine A, Katano Y, Nishimura T, Kato Y, et al. Sonographic evaluation of the peripheral nerve in diabetic patients: the relationship between nerve conduction studies, echo intensity, and cross-sectional area. J Ultrasound Med 2010;29:697-708.
18. Tagliafico A, Tagliafico G, Martinoli C. Nerve density: a new parameter to evaluate peripheral nerve pathology on ultrasound. Preliminary study. Ultrasound Med Biol 2010;36:1588-1593.
19. Ghasemi-Esfe AR, Khalilzadeh O, Vaziri-Bozorg SM, Jajroudi M, Shakiba M, Mazloumi M, et al. Color and power Doppler US for diagnosing carpal tunnel syndrome and determining its severity: a quantitative image processing method. Radiology 2011;261:499-506.
20. Sernik RA, Abicalaf CA, Pimentel BF, Braga-Baiak A, Braga L, Cerri GG. Ultrasound features of carpal tunnel syndrome: a prospective case-control study. Skeletal Radiol 2008;37:49-53.
21. Erel E, Dilley A, Greening J, Morris V, Cohen B, Lynn B. Longitudinal sliding of the median nerve in patients with carpal tunnel syndrome. J Hand Surg Br 2003;28:439-443.
22. Wang Y, Filius A, Zhao C, Passe SM, Thoreson AR, An KN, et al. Altered median nerve deformation and transverse displacement during wrist movement in patients with carpal tunnel syndrome. Acad Radiol 2014;21:472-480.
|
|
||||||||||||||||||||||||||||||||||