Hashimoto’s encephalopathy (HE) is a rare neurological disorder with clinical manifestations that vary between patients. This clinical diversity makes diagnosis difficult, and leads to frequent misdiagnoses. Symptoms of HE include disorders of consciousness, impairment of cognitive function, confusion, stroke-like episodes, and seizures.1,2 HE can be divided into two subtypes: 1) HE with diffuse encephalopathy that shows encephalopathic symptoms without focal neurological abnormalities, and 2) HE with focal encephalopathy that shows focal neurological abnormalities. However, high antithyroid antibody levels and responsiveness to immunotherapy are common in both HE subtypes.2 Electroencephalography (EEG) findings also vary between individual patients and may also depend on the clinical stage of the disease.3 Here we describe a patient with HE who displayed symptoms mimicking infectious encephalitis such as fever, aphasia, and focal EEG abnormality. We also discuss the possible pathomechanisms and clinical significance of HE.
CASE
A 69-year-old woman with diabetes visited the emergency department of the author’s hospital with sudden-onset confusion and aphasia. These symptoms began during a telephone call with an acquaintance, where the patient suddenly forgot who she was talking to and responded inadequately. The acquaintance recommended for the patient to consume orange juice, but after her symptoms had persisted for longer than 3 hours she decided to visit a hospital. At presentation her vital signs were stable except for a fever of 39.1°C, while a neurological examination showed confusion with impaired comprehension, repetition, and naming without other focal neurological abnormalities. Her body temperature fluctuated between 37.5°C and 39.0°C over a 10-hour period, which was intermittently controlled by administering acetaminophen. The confusion with aphasia persisted after admission.
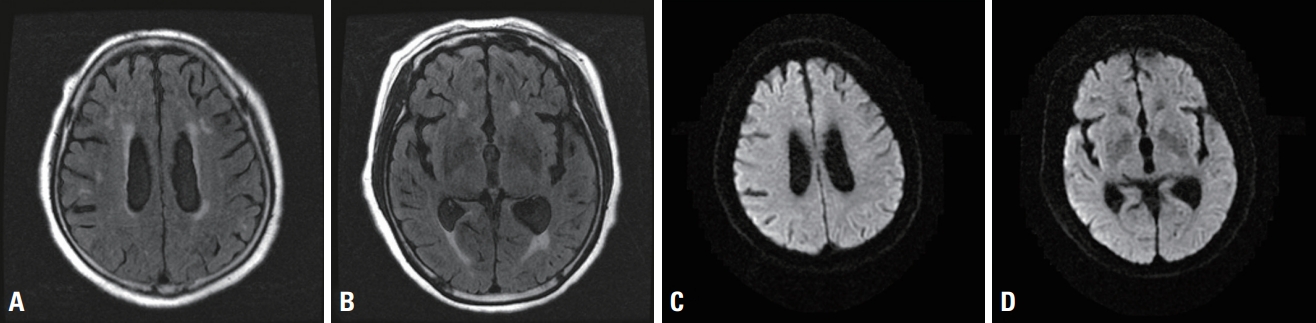
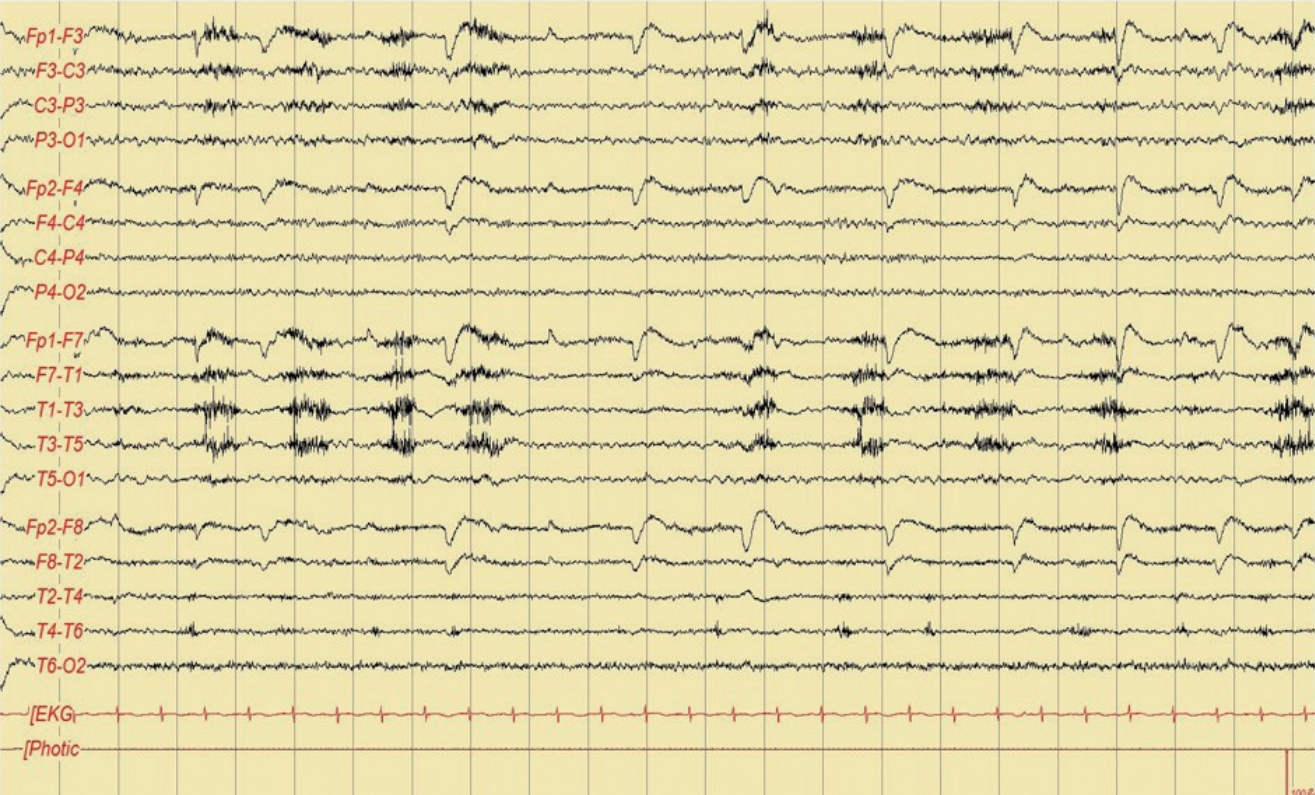
Tests for the blood count, erythrocyte sedimentation rate, liver and kidney functions, coagulation screening, C-reactive protein, serum electrolytes, urinalysis, and antinuclear antibody yielded normal results. Magnetic resonance imaging that included fluid-attenuated inversion recovery and diffusion-weighted imaging modalities revealed no significant abnormality (Fig. 1). EEG performed on the day after admission showed intermittent rhythmic and quasi-rhythmic slow waves with a fluctuating frequency in the left hemisphere (Fig. 2).
Based on the above-described clinical and EEG manifestations, we performed a cerebrospinal fluid (CSF) test to exclude the possibility of infectious encephalitis. However, the CSF examination revealed no pleocytosis, and her CSF protein and glucose levels were within the reference limits (45 mg/dL and 64 mg/dL, respectively). Polymerase chain reaction analysis for Mycobacterium tuberculosis and herpes simplex virus also produced negative results. No specific inflammatory lesion or tumor was observed on computed tomography (CT) scans of her chest and abdomen, and no bacterial or fungal growth was observed in the sputum, blood, urine, or CSF culture. While a thyroid function test showed no specific abnormality, the levels of antibodies against thyroperoxidase were significantly higher (>1,300 IU/mL) than the normal value of <60 IU/mL.
Valproic acid was administered intravenously at a loading dose of 1,000 mg followed by a maintenance dose of 250 mg twice daily from the second day of admission. Her fever subsided after the antiepileptic treatment, while her cognitive symptoms improved considerably. However, mild confusion and incomprehension still persisted despite the disappearance of focal epileptic discharges in the EEG performed 4 hours after the initial EEG (Fig. 3). The patient’s score on the Korean version of the Mini Mental State Examination (K-MMSE) was 16 on the third day of admission. After administering oral prednisolone at 30 mg once daily from the fifth day of admission, she gradually recovered to her premorbid state. Her K-MMSE score was 26 on the tenth day. The aphasia and confusion had not recurred up to the time of discharge at 3 months after initiating low-dose medication of prednisolone (5 mg once daily) and valproic acid (250 mg twice daily).
DISCUSSION
HE is a rare but very serious disease. Its incidence and prevalence have not been elucidated due to diagnosis difficulties associated with the absence of specific clinical features and/ or neuroimaging findings.2 Despite high titers of antithyroid antibodies observed in patients, the thyroid function test shows little to no abnormality.1,2 Clinical suspicion is the only helpful method for an early diagnosis, which is crucial for preventing the significant neurological sequelae. Definitive diagnostic criteria for HE have not been established, but the following criteria are commonly applied: clouding of consciousness with reduced wakefulness, attention, or cognitive function; no evidence of CSF infection; and a high concentration of antithyroid antibodies (microsomal, thyroperoxidase, or thyroglobulin antibodies).2 Applying these criteria meant that the clinical and laboratory findings in our patient were compatible with HE.
Cases of fever caused by HE are rare. Fever may be caused by complications such as aspiration pneumonia or urinary tract infection in patients with altered mentality. However, despite our patient presenting with a fever, bacterial growth was not observed in the blood, sputum, or urine culture. Furthermore, no inflammatory lesion was observed on CT scans. There is only one case report of febrile HE in the literature, and the underlying mechanism remains unclear.4 One possible mechanism is that the increased tumor necrosis factor-a observed in autoimmune thyroiditis acts as an endogenous pyrogen in patients with HE.5 Another possible mechanism is that the fever is associated with complex partial seizures; this is because the hypothalamic thermoregulatory center is thought to be involved during seizure propagation and may act as a symptomatogenic zone.6-8 The fever in our patient subsided after applying antiepileptic treatment. Therefore, while both mechanisms may contribute to febrile episodes, the latter mechanism seemed to be a more likely cause for the fever observed in our patient.
The EEG findings in our patient showed rhythmic and quasi-rhythmic slowing with fluctuation in the left hemisphere. No definite evolution in the pattern (increase in voltage with increase or decrease in frequency) or location was observed in the EEG of our patient. However, the fluctuation of rhythmic and quasi-rhythmic discharges was abolished after administering an antiepileptic drug, which meets the diagnostic EEG criteria for nonconvulsive status epilepticus (NCSE).9 Short-acti benzodiazepine is commonly used for detecting EEG changes and diagnosing NCSE. However, intravenous valproic acid can be substituted for benzodiazepine because its concentration peaks within a few minutes and so EEG changes can be detected rapidly after its administration.
EEG findings may also lead to the misdiagnosis of HE as an infectious encephalitis such as herpes simplex encephalitis (HSE) due to focal epileptiform discharges with focal slowing typically being found in patients with HSE.10 However, unlike HSE, the EEG traces of HE are heterogeneous, with focal, generalized slowing, periodic discharges, or even triphasic waves typical of metabolic encephalopathy.4 Confirming a diagnosis of febrile HE showing focal EEG abnormalities therefore requires a CSF examination in order to exclude the possibility of HSE.
In conclusion, diagnosing febrile HE is challenging, and necessitates CSF analysis and antithyroid antibody tests to ensure accuracy. After excluding infectious encephalitis, the early administration of corticosteroids and controlling the seizures associated with HE are crucial interventions for successful treatment. Furthermore, the concentration of antithyroid antibodies should be checked when diagnosing HE, even in patients showing focal encephalopathy with fever.